54 years female with pneumonia long case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
Daily routine:
She is a farmer by occupation.
Wakes up at around 7:00 am in the morning. Eats breakfast by 8:00 am. Goes to his farm and monitors work. Then comes back to his house in the afternoon and has lunch by 1:00 pm. Sleeps for a while in the afternoon
He has a cup of tea in the evening at around 5:00 pm , watches TV for a while and has dinner at around 8:00 pm and goes to bed at around 9:30 pm.
Chief complaints:
patient was brought to the casualty with c/o cough and sputum
HOPI:
Patient was apparently asymptomatic 1 month ago the she developed fever which was low grade intermittent and incidious in onset and was gradually progressing and relieved on taking medication
Fever increasesd gradually from past 4 days which was associated with generalised weakness and body pains
H/o dysnea which was incidious in onset and gradually progressive patient also gives history of pain in the epigastric region on inspiration
No h/o chest pain , palpitations , swetting
No h/o nausea, vomiting and loose stools
HISTORY OF PAST ILLNESS:
Patient was diagnosed with hypertension 6 months ago and he is on medications
Patient also gives the history of pain in multiple small joints of hand , knee and shoulders since 10 yrs and used aurvedic medicine
Not a k/c/o type 2 DM , astham , thyroid disorder
Personal history:
Diet : mixed
Appetite : decreased
Bowel movement: regular
Bladder movments : normal
Habits: has a habit of consumption of toddy occasionally
Patient also has a habit of cheweing betal leaf
FAMILY HISTORY :
No significant family history
Treatment history:
Patient is on hypertensive drugs since 6 months
General examination:
Patient is conscious, coherent and cooperative
Patient was examined in well lit room after taking well informed consent.
No /icterus/cyanosis/clubbing/Generalized lymphadenopathy
Pallor(+)
VITALS ON ADMISSION -
BP : 140/90 mm hg
PR : 106bpm
temparature: 102.7 f
RR :30 cpm
GRBS: 140 mg
SYSTEMIC EXAMINATION:
Cvs : S1 s2 heard no murmurs
RS : BAE+
Vesicular breath sounds , dyspnea (+)
Wheeze(-)
CNS examination:
Concious
Speech:normal
Gait: normal
Sensory system :normal
Motor system: normal
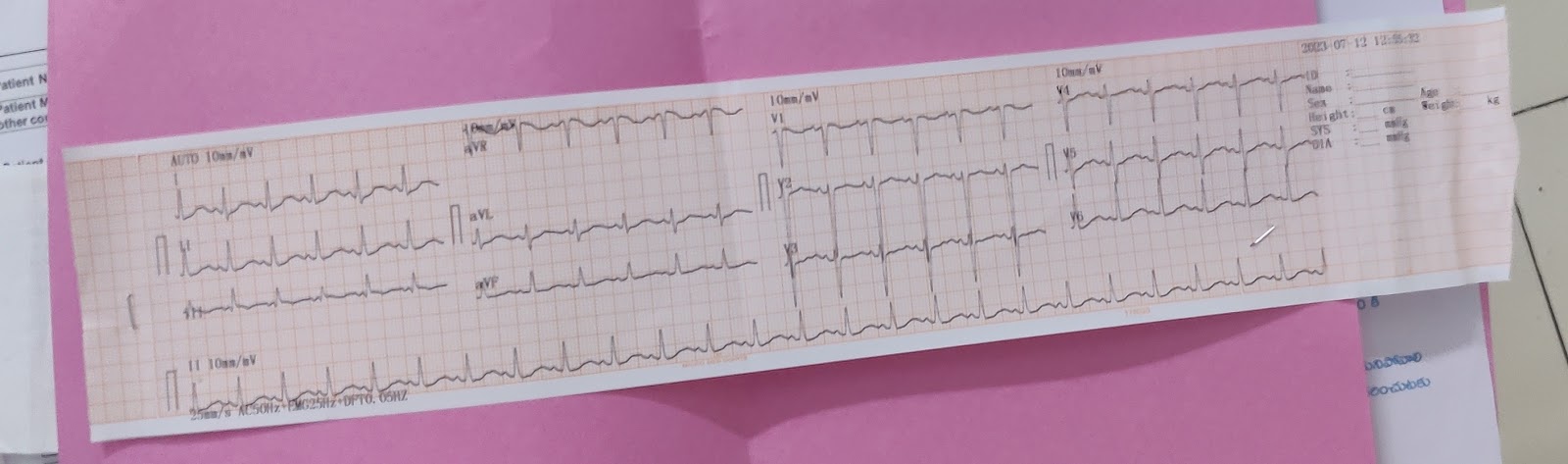
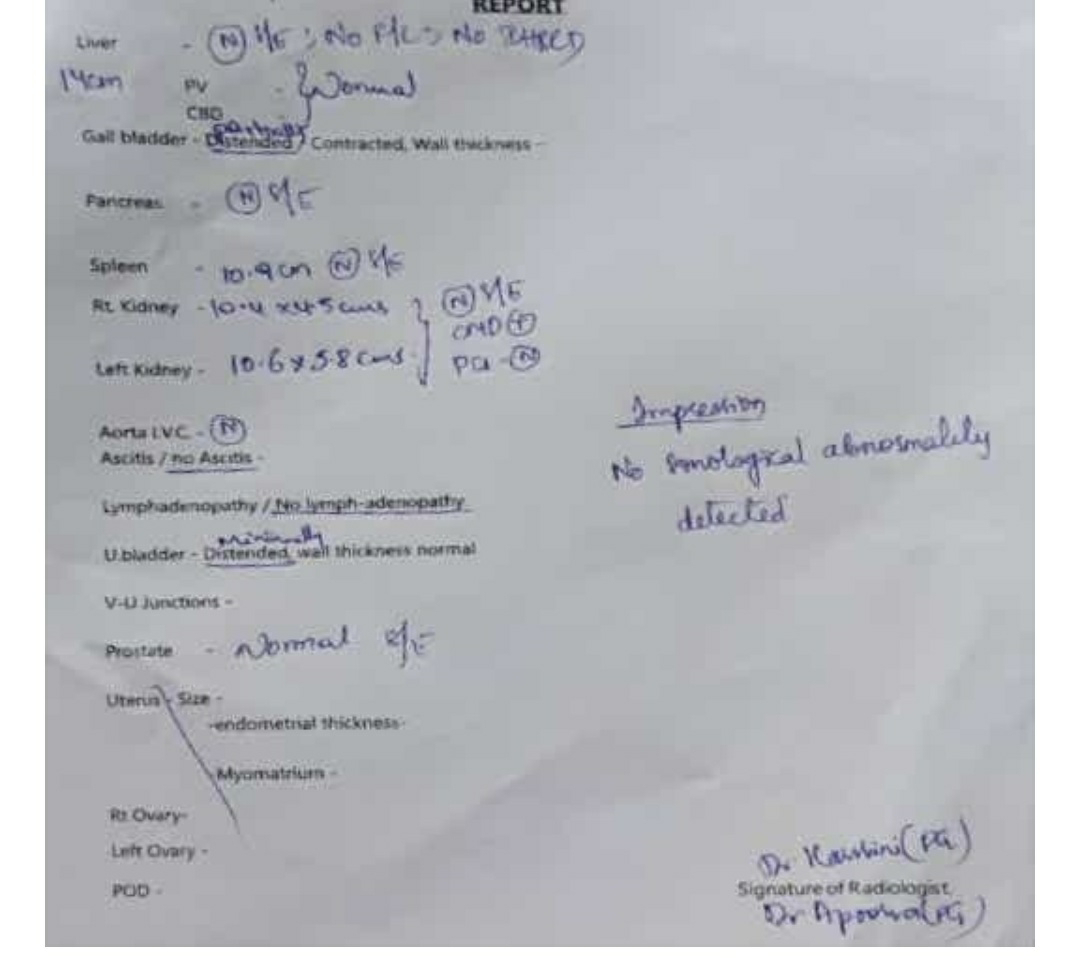
INVESTIGATIONS:
TREATMENT :
INJ. LASIX 40mg iv/bd
INJ.NEOMOL 1gm IV/ sos if temp > 101°F
TAB . AZITHROMYCIN 520mg /po/od
TAB . AGUMENTIN 625 mg /po/od
Srup . Ascoril 10 ml /po/od
Provisional diagnosis :
Pneumonia, CAD






Comments
Post a Comment