A 63 year old male with burning sensation with epigastrium patient compliants with constipation and incomplete evacuvation of stools
This is an online elog book to discuss our patients de-identified health data shared after taking his/her/guardians signed informed consent.Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This elog book reflect s my patients centered online portfolio and your valuable inputs on the comments is welcome
Date of admission:16/01/23
Chief complaints:
63years old male patients with chief complaints of constipation and incomplete evacuvation of stools since 3 years
History of present illness:
Patient was apparently asymptomatic 3 years back then he developed incomplete passage of stools since 3 years
Passes stools twice a day and no history of hard stools and complaints of low abdomen pain at night relieves spontaneously during day time and associated with bloting sessation since 1 year and buring type of chest pain no radiation of pain no sob no history of pain on defecation staring on passing of stools constipation altering diarrhoea and no history of malabsoption
History of past illness:
Patient is a k/c/o hypertension since 1 year and is on regular medication
Patient is not a know case of diabetics, epilepsy,tb,asthma
Tab : Telmisartan40mg
Tab:Amilodipine5mg
History of scabies since1 year ( resolved now)
Family history:
No known relavent family history
Personal history:-
Diet- vegitarian
Apetite- normal
Sleep- normal
Bowel movements- regular
Addictions-ciggrates or beedi daily since 20 year
General examination:-
Patient is conscious, coherent, cooperative,well oriented to time, place and person.
No sign of pallor, icterus, clubbing, cyanosis,
Drug and allergic history
No known relavent drug history
Vitals
Temperature: afebrile
Pulse rate:70bpm
Bp:130/80 mm/hg
Respiratory rate:23 cpm
SpO2:98
Systemic examination
ABDOMEN:
INSPECTION: Shape:scaphoid
Spleen : Non palpable
Liver: non palpable
Tender: non palpable
Umbilicus: central &everted
no scars,no scratches, normal hernial orrifice
PALPATION: soft ,nontender
AUSCULTATION: bowel sounds heard
CVS:
S1&S2 heard
no murmurs
CNS:
Concious
Speech:normal
Gait: normal
Sensory system :normal
Motor system: normal
Provisional diagnosis: constipation and irritabel bowel syndrome symptoms
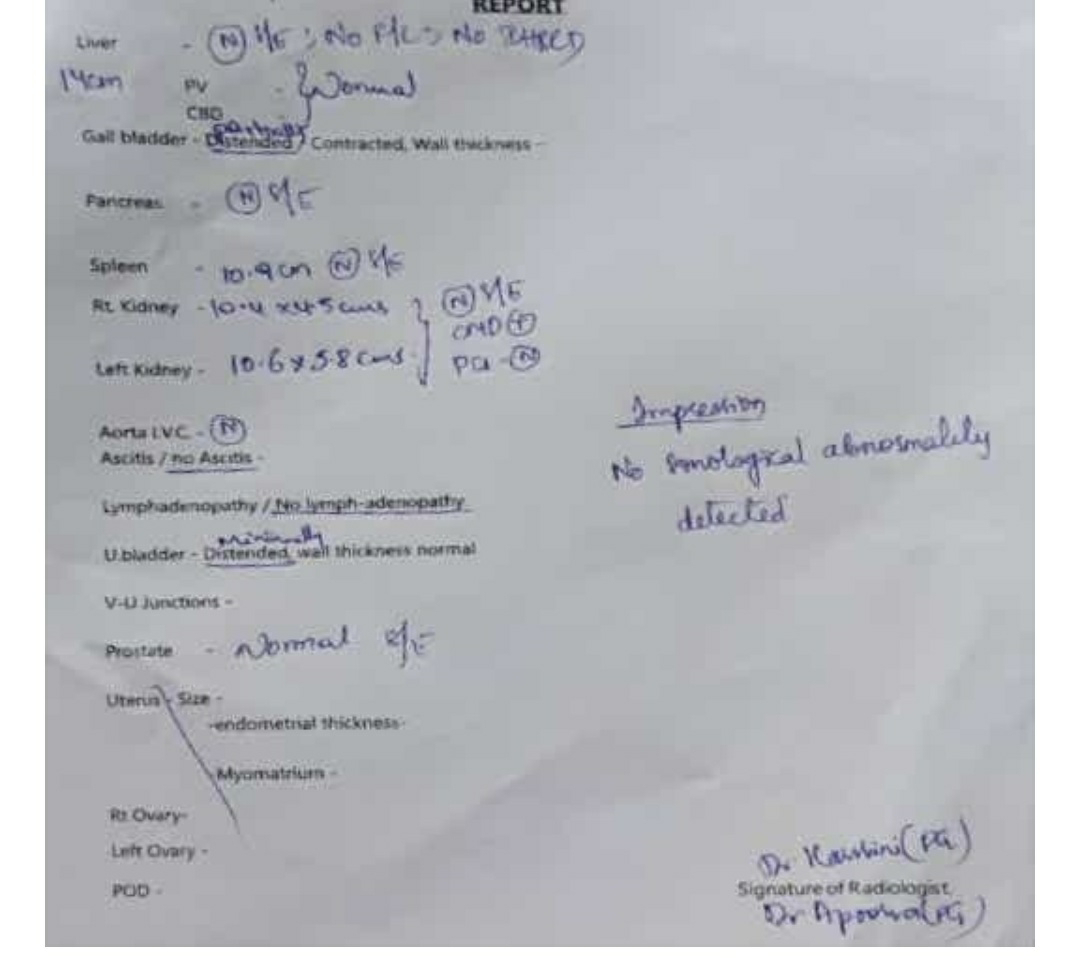
INVESTIGATIONS:
TREATMENT:
TAB : pan40mg PO OD
TAB : telmisartan 40mg + amlodipine 5 mg
FINAL DIAGNOSIS: burning sensation in epigastrium






Comments
Post a Comment