63 year old male with sob and pedal edema
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
Daily routine:
He is a farmer by occupation.
Resident of Miryalagudem
Stopped working 2 years ago due to right femur fracture and old age.
Wakes up at around 7:00 am in the morning. Eats breakfast by 8:00 am. Goes to his farm and monitors work. Then comes back to his house in the afternoon and has lunch by 1:00 pm. Sleeps for a while in the afternoon
He has a cup of tea in the evening at around 5:00 pm , watches TV for a while and has dinner at around 8:00 pm and goes to bed at around 9:30 pm.
Chief complaints:
Patient was brought to casualty with c/o shortness of breath Grade III MMRC since 20 days
HOPI
Patient was apparently asymptomatic 1 year ago when he developed chest pain and SOB Grade III and went to a hospital in Hyderabad
Presently- on 9/7/23
20 days back he developed Shortness of breath Insidious in onset , initially Grade I and gradually progressed to Grade-III.
It was associated with Right sided chest pain , non radiating , pricking type of pain
It was also associated with PND, dry cough and sweating
No c/o orthopnea, palpitations and giddiness
Patient also C/o B/L lower limbs swelling since 5-6 months, pitting type, extending upto the knee, aggravated on sitting, standing and walking and relieved on lying down.
Patient also complains of decreased urine output and facial puffiness since 3 days
He also complains of constipation- passes stools every 3-4 days.
He also has distended abdomen since 3 days
No c/o pain abdomen, vomitings, fever, cough, cold
PAST HISTORY -
Patient is k/c/o DM 2 since 5 years and is on regular medication - Tab. Metformin 500 mg BD
He is also a k/c/o Hypertension since 5 years and is on regular medication - Tab. Metoprolol 25 mg + Tab. Amlodipine 5mg OD
H/o CAD 1 year ago - underwent Percutaneous Transluminal Coronary Angioplasty with 3 stents- done along with Tab. Atorvas 10mg + Tab. Clopidogrel 75 mg.
Not a k/c/o TB, Asthma, Epilepsy, Thyroid disorders and CVA.
H/o Right femur fracture 2 years years ago, underwent open reduction and internal fixation.
Underwent Knee replacement for Left knee 7 years ago.
PERSONAL HISTORY:
Diet: Mixed
Appetite: Normal
Sleep: Adequate
Bladder: Decreased urine output.
Bowel : Constipation+ (Passes stools once in 3-4 days )
Patient was an alcoholic and cigarette smoker for about 15 years.
Stopped alcohol 10 years ago.
Stopped smoking 20 years ago.
No known allergies
FAMILY HISTORY:
No significant family history
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative
Patient was examined in well lit room after taking well informed consent.
Patient is moderately built and moderately nourished
Pitting edema Grade III present.
No pallor/icterus/cyanosis/clubbing/Generalized lymphadenopathy
VITALS ON ADMISSION -
Temp: Afebrile
PR: 88 bpm
RR: 17 cpm
BP: 130/80mmHg
Spo2: 87% @RA
GRBS: 202 mg/dl
SYSTEMIC EXAMINATION:
CVS: S1 S2 heard, No murmurs
RS: BAE+, crepitations -in Left IAA
P/A: Distended, non tender
Umbilicus -
No engorged veins, scars or sinuses
1. Autonomic function: Normal
2. CNS examination:
Pupils -B/L NSRL
GCS - E4V5M6
Cranial nerves - NAD
MOTOR SYSTEM :
Rt Left
Bulk: N. N
Tone: Rt Left
UL. N N
LL. N N
Deep tendon reflexes:
Biceps: +2 +2
Triceps: +2 +2
Supinator: +1 +1
Knee: +2. +2
Ankle: +2 +2
Plantar: flexor B/L
Sensory system : Intact
PROVISIONAL DIAGNOSIS -
?Heart failure ?COPD
INVESTIGATIONS on 9/7/23-
ECG-
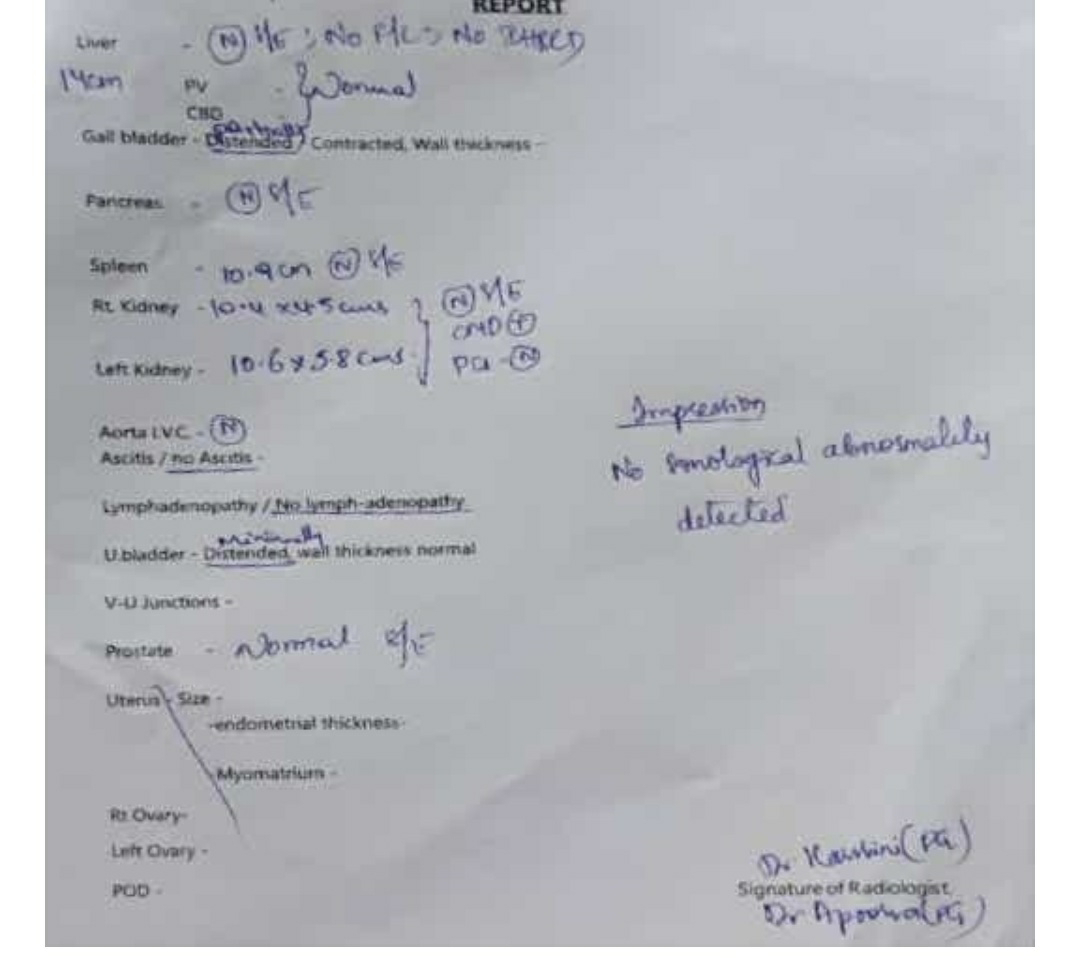
USG abdomen -
Chest X-Ray:PA view
Hemogram -
Hb: 9.6 gm/dl
TLC: 8,100
N/L/E/M/B - 75/15/ 1/10/0
RBC - 3.77
Platelets :3.30
PBS:NC/NC
RBS - 148 mg/dl
Urea: 41 mg/dl
Creatinine: 1.2
Na: 143
K: 4.3
Cl: 98
Ca (ionized)- 1.12
Total bilirubin - 1.39
Direct bilirubin - 0.29
AST- 27
ALT - 24
ALP - 141
Total protein - 5.8
Albumin 3.16
A/G: 1.20
CUE: Albumin +
Sugar- ++++
Ep cells - 5-6
Pus cells -2-4
HBsAG - negative
HCV- negative
HIV 1/2 -negative
TREATMENT:
1) INJ. LASIX 50 MP IV/BD
2) TAB. METFORMIN 500MG PO/BD
3) TAB. AMLONG MT 5/25 MG PO/OD
4) TAB. ATOCOR CV 10 PO/ OD
5) TAB. PULMOCLEAR 100/600MG PO/BD
6) SYP. ASCORIL D 10ML PO/TID
7) NIV
8) LASIX INFUSION AT 5ML / HOUR
9) TAB RAMIPRIL 2.5 MG PO/OD
10/07/2023
S:
2 fever spikes at 4 and 6 am
SOB and cough decreased
O:
Patient is conscious coherent and cooperative
No icterus,cyanosis,clubbing,
lymphadenopathy
Bp-120/80mmHg
Pr- 92 bpm
Temperature - Afebrile
Rr- 19 cpm
Spo2- 92% on RA
Grbs- 149mg/dl @8am
I/o-240/2600 ml
CVS-S1,S2 heard ,no murmurs
RS- BAE present
NVBS ,Mild crepts in Left IAA
CNS-
Pupils- B/L NSRL
GCS - E4V4M6
Deep tendon reflexes:
Biceps: +2 +2
Triceps: +2 +2
Supinator:. + +
Knee: +2 +2
Ankle: +2 +2
Plantar: flexor flexor
P/A- Soft, NT
A:
SOB UNDER EVALUATION
?HEART FAILURE
?COPD
K/C/O HTN AND DM II SINCE 6 YEARS
S/P : PTCA 1 YEAR AGO
P:
1. Intermittent NIV
2. Inj. Lasix infusion @2.5ml per hour
3. Tab. Metformin 500 mg PO/BD
4. Tab. Amlodipine 5 mg + Metoprolol 25 mg PO/OD
5. Tab. Atorvas - CV PO/OD
6. Tab. Ramipril 2.5 mg PO/OD
7. Tab. Pulmoclear 100/600 mg PO/BD
8. Tab. Ascoryl 10 ml PO/ TID


Comments
Post a Comment