42 years old male patients with chief complaints of fever and headache since 5 days
- Get link
- X
- Other Apps
This is an online elog book to discuss our patients de-identified health data shared after taking his/her/guardians signed informed consent.Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This elog book reflect s my patients centered online portfolio and your valuable inputs on the comments is welcome
Date of admission:9/12/22
Chief complaints:
42 years old male patients with chief complaints of fever and headache since 5 days
History of present illness:
Patient was apparently asymptomatic 5 days back then he developed fever of low grade which reduced on taking medication
Fever was associated with headache which was pricking type.
Patient was diagnosed with renal failure
History of past illness:
Patient is a k/c/o hypertension since 1 year and is on regular medication
Patient is not a k/c/o diabetes, epilepsy, asthma, cad
Family history:
Patient mother had hypertension
Personal history:-
Occupation-daily wage labourer
Diet- mixed
Apetite- lost
Sleep-disturbed
Bowel movements- normal
Addictions-alcohol consumption and beedi daily 1 pack since 15years of age
General examination:-
Patient is conscious, coherent, cooperative,well oriented to time, place and person.
No sign of pallor, icterus, clubbing, cyanosis,
Generalized lymphedenopathy
Vitals:-
Temp- 98 F
Bp-160/100mm hg
PR- 76pm
RR-16cpm
Systemic examination:-
Cvs-S1 S2 heard, no murmurs heard
RS- bae+ ,normal vesicular breath sounds
Abdomen-scaphoid, liver spleen not palpable
CNS:Conscious,
Slurred speech
Signs of meningeal irritation-
Neck stiffness is present
Kernigs sign absent
Tone of upper limbs is normal, Hypertonia in right lower limb
Power upper limbs right 5/5 and left - 5/5 and lower right limb 4+/5 lower left limb - 4+/5
CRANIAL NERVE intact
RIGHT: Biceps +3
Triceps+3
Supinator+2
Knees+3
Ankle+2
LEFT: Biceps +2
Triceps +2
Supinator +2
Knees +2
Ankle +1
Cerebellar signs:
Finger to nose coordination is absent
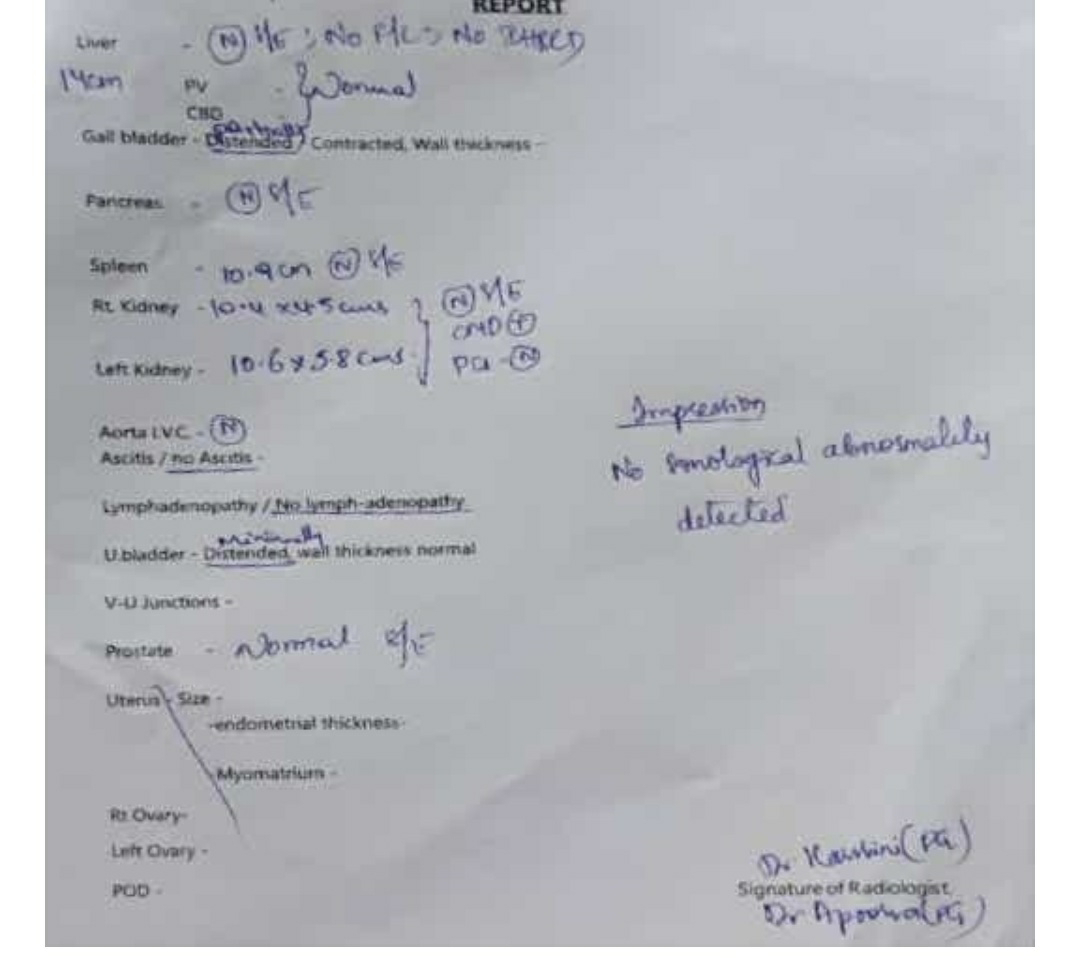
Clinical images
Investigations:
Provisional diagnosis:
AKI
?meningitis
Treatment:
IVF ns 50ml/hr
Tab cinod 10mg po
Popular posts from this blog
A 45 year old woman complaints of lower back pain and neck pain
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome . CHIEF COMPLAINTS: A 45years old woman came to OPD with chief complaints of neck pain on and off since 6 years when she feels that she has high sugars and pain radiating towards shoulders causing headache. She also complaints of Low back pain on and off since 2 to 3 years only when she is sitting for long hours. HISTORY OF PRESENT ILLNESS Patient is a k/c/o Type 2 diabetes mellitus diagnosed 6 years ago. Patient had c/o polyuria 6 years back then got on routine investigation, she
60 year old male patient pedal edema and decreased urine output since 1 month
This is an online elog book to discuss our patients de-identified health data shared after taking his/her/guardians signed informed consent.Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This elog book reflect s my patients centered online portfolio and your valuable inputs on the comments is welcome. 60 year old male patient came with chief complaints of pedal edema and decreased urine output since 1 month PERSONAL HISTORY •He is married •Appetite normal •Mixed diet •Bowel movement regular •Micturiton abnormal decreased urine output •No known allergies and addictions FAMILY HISTORY No history of diabetes, hypertension, heart disease, stroke, tuberculosis, asthma ON EXAMINATION •Patient is conscious, coherent, co-operative •Pallor, icterus, clubbing, cyanosis, lymphadenopathy are absent. •Oedema of feet is
- Get link
- X
- Other Apps















Comments